1801006014 -.LONG CASE
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centred online learning portfolio and your valuable inputs on the comment box is welcome."I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan .
No similar complaints in the family.
Power:-
Rt UL - 3/5 Lt UL-5/5
Rt LL - 3/5 Lt LL-5/5
Tone:-
Rt UL - Increased
Lt UL- Normal
Rt LL- Increased
Lt LL- Normal
Reflexes:
Right Left
Biceps: +++ ++
Triceps: +++ ++
Supinator: +++ ++
Knee: +++ ++
Ankle: +++ ++
Plantar: Muted Flexion
Involuntary movements - absent
Fasciculations - absent
Sensory system -
-Pain, temperature, crude touch, pressure sensations normal
-Fine touch, vibration, proprioception normal
-two point discrimination -able to discriminate and tactile localisation -able to localise
Cerebellum -
Finger nose test normal, no dysdiadochokinesia, Rhomberg test could not be done
Gait:
ABDOMEN EXAMINATION:
Inspection -
Umbilicus - inverted
All quadrants moving equally with respiration
No scars, sinuses and engorged veins , visible
pulsations.
Palpation -
soft, non-tender
no palpable spleen and liver
Percussion - live dullness is heard at 5th intercoastal space
Auscultation- normal bowel sounds heard.
CARDIO VASCULAR SYSTEM:
Inspection :
Shape of chest- elliptical
No engorged veins, scars, visible pulsation
Palpation :
Apex beat can be palpable in 5th inter costal space
No thrills and parasternal heaves can be felt
Auscultation :
S1,S2 are heard
no murmurs
RESPIRATORY SYSTEM:
Inspection:
Shape- elliptical
B/L symmetrical ,
Both sides moving equally with respiration .
No scars, sinuses, engorged veins, pulsations
Palpation:
Trachea - central
Expansion of chest is symmetrical.
Vocal fremitus - normal
Percussion: resonant bilaterally
Auscultation:
bilateral air entry present. Normal vesicular breath sounds heard.
PROVISIONAL DIAGNOSES:
Cerebrovascular accident with Right sided hemiparesis due to involvement of posterior limb of internal capsule.
INVESTIGATIONS:
INVESTIGATIONS
•13/3/2023
*Blood sugar random - 109 mg/dl
*FBS - 114 mg/dl
*Complete blood picture:
Hemoglobin- 13.4 gm/dl
WBC-7,800 cells/cu mm
Neutrophils- 70%
Lymphocytes- 21%
Esinophils- 01%
Monocytes- 8%
Basophils- 0
PCV- 40 vol%
MCV- 89.9 fl
MCH- 30.1 pg
MCHC- 33.5%
RBC count- 4.45 millions/cumm
Platelet counts- 3.01 lakhs/ cu mm
*SMEAR:
RBC - normocytic normochromic
WBC - with in normal limits
Platelets - Adequate
Haemoparasites - no
*CUE:
Colour - pale yellow
Appearance- clear
Reaction - acidic
Sp.gravity - 1.010
Albumin - trace
Sugar - nil
Bile salts - nil
Bile pigments - nil
Pus cells - 3-4 /HPF
Epithelial cells - 2-3/HPF
RBC s - nil
Crystals - nil
Casts - nil
Amorphous deposits - absent
*LFTs:
Total bilirubin - 1.71 mg/dl
Direct bilirubin- 0.48 mg/dl
AST - 15 IU/L
ALT - 14 IU/L
Alkaline phosphatase - 149 IU/L
Total proteins - 6.3 g/dl
Albumin - 3.6 g/dl
A/G ratio - 1.36
*Blood urea - 19 mg/dl
*Serum creatinine - 1.1 mg/dl
*Electrolytes
Sodium - 141 mEq/L
Potassium - 3.7 mEq/L
hloride - 104 mEq/L
Calcium ionised - 1.02 mmol/L
*Anti HCV antibodies rapid - non reactive ;
*HIV 1/2 rapid test - non reactive
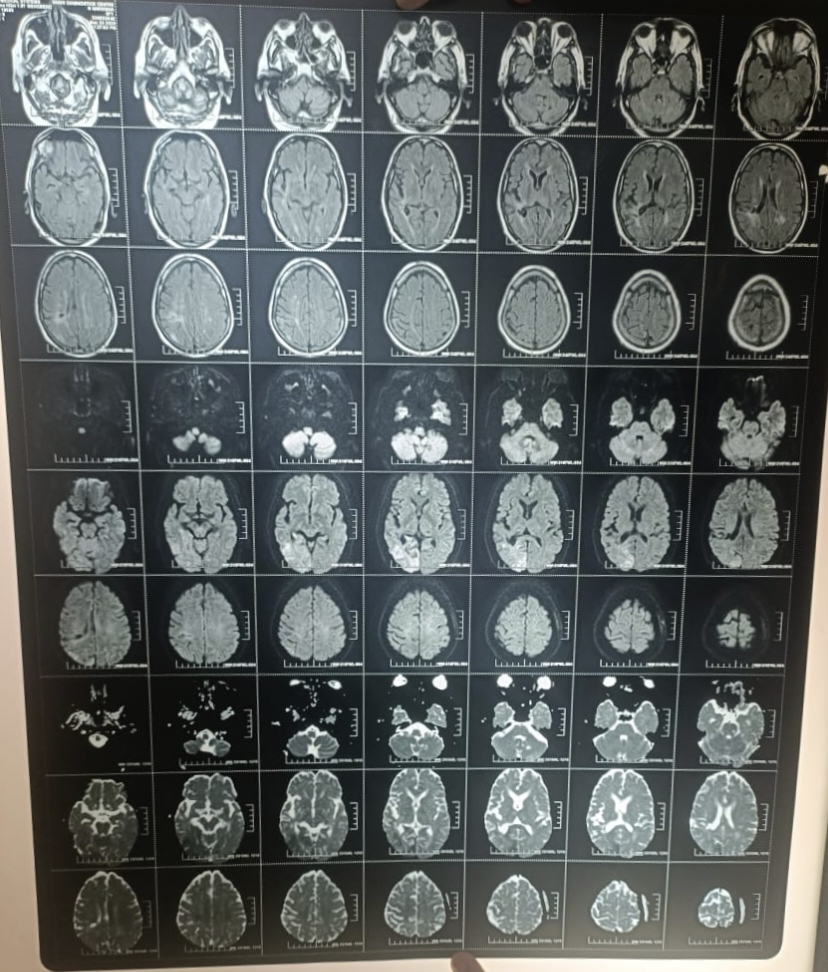
*MRI





















Comments
Post a Comment