27 years male with CLD
This is an online E-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient centered online learning portfolio and your valuable comments on comment box is welcome.
I've been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CASE:
27 years old male , resident of nalgonda,came to OPD with chief complaints of loss of appetite since 20 days
Complains of tremors since 15 days
Complains of blood in urine since 10 days
Complains of pedal edema since 10 days
HISTORY OF PRESENT ILLNESS
Patient was apparently asymptomatic 20 days back then he had loss of appetite for which he went to hospital and diagnosed as CLD, splenomegaly with portal hypertension and took medication. After which he complains of hematuria since 10 days and pedal edema which is pitting type, relieved on taking rest and aggravated on walking. Has tremors since 15 days. Malena positive 20 days back for 10 days.
No abdominal pain, no vomitings, no burning micturition, no loose stools.
PAST HISTORY
H/O surgery appendectomy
N/k/c/o HTN,DM, TB,CVD, thyroid disorders ,epilepsy.
PERSONAL HISTORY:
Diet - mixed
Appetite - increased
Sleep -adequate
Bowel and bladder movements - regular
Addictions- Alcohol consumption since 7 years, whisky (500ml) daily.
DAILY ROUTINE:
4am- wake up
8:00 -8:30 am - breakfast
1pm-3pm - lunch
7:30pm-8:30pm - drinks alcohol
9pm - dinner
FAMILY HISTORY :
Not significant
GENERAL PHYSICAL EXAMINATION:
Patient is conscious, coherent and cooperative.
Moderately build and nourished.
Pallor -absent
Icterus- present
Clubbing- absent
Cynosis- absent
Lymphadenopathy -absent
Pedal Edema -present
Tremors:
Vitals:
Temp:- 97.6
PR- 95 bpm
BP- 100/60 mmHg
Spo2-95% at room Air
GRBS- 75mg%
SYSTEMIC EXAMINATION:
CVS- S1s2present, no murmurs heard
RS-B/L air entry present
N vesicular breath sounds
PA- soft,NT
CNS - NFND
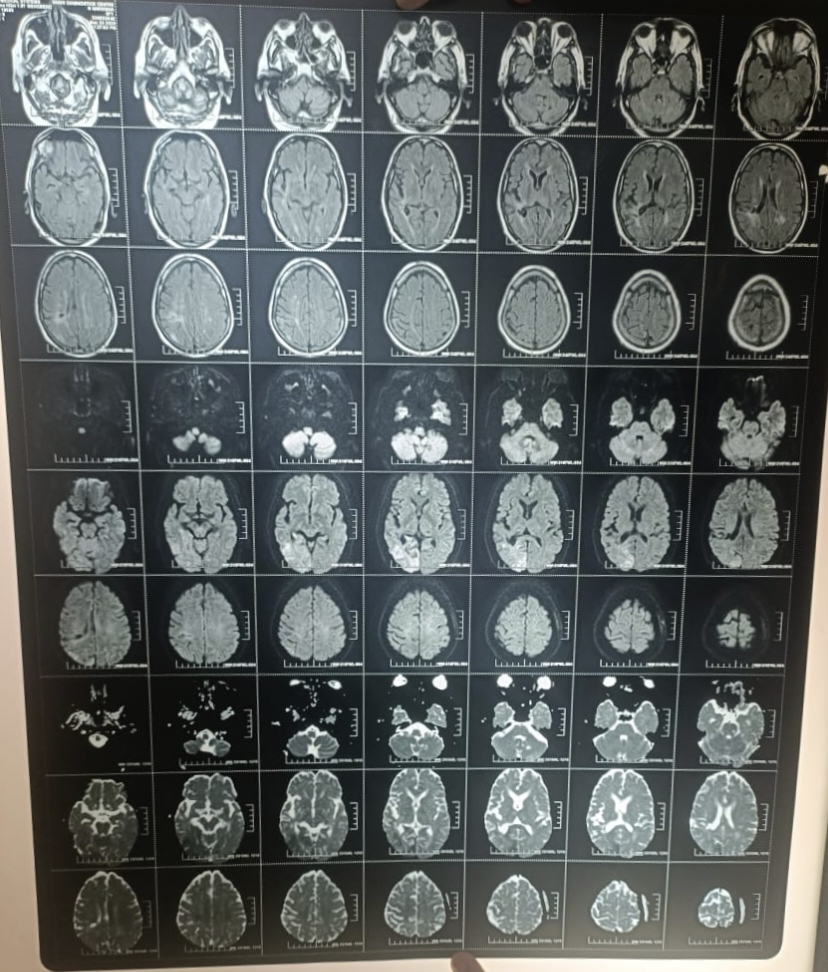
INVESTIGATIONS:

DECOMPENSATED LIVER DISEASE - grade 1 ( hepatic encephalopathy)
HYPOTONIC HYPONATREMIA - diuretic induced



















Comments
Post a Comment